Overview
Cardiomyopathy (kahr-dee-o-my-OP-uh-thee) is a disease of the heart muscle that makes it harder for the heart to pump blood to the rest of the body. Cardiomyopathy can lead to heart failure.
The main types of cardiomyopathy include dilated, hypertrophic and restrictive cardiomyopathy. Treatment — which might include medications, surgically implanted devices, heart surgery or, in severe cases, a heart transplant — depends on the type of cardiomyopathy and how serious it is.
Types
Symptoms
There might be no signs or symptoms in the early stages of cardiomyopathy. But as the condition advances, signs and symptoms usually appear, including:
- Breathlessness with activity or even at rest
- Swelling of the legs, ankles and feet
- Bloating of the abdomen due to fluid buildup
- Cough while lying down
- Difficulty lying flat to sleep
- Fatigue
- Heartbeats that feel rapid, pounding or fluttering
- Chest discomfort or pressure
- Dizziness, lightheadedness and fainting
Signs and symptoms tend to get worse unless treated. In some people, the condition worsens quickly; in others, it might not worsen for a long time.
When to see a doctor
See your health care provider if you have one or more signs or symptoms associated with cardiomyopathy. Call 911 or your local emergency number if you have severe difficulty breathing, fainting or chest pain that lasts for more than a few minutes.
Some types of cardiomyopathy can be passed down through families (inherited). If you have the condition, your health care provider might recommend that your family members be checked.
Causes
Dilated cardiomyopathy

Dilated cardiomyopathy
Dilated cardiomyopathy causes the chambers of the heart to grow larger. Untreated, dilated cardiomyopathy can lead to heart failure.
Hypertrophic cardiomyopathy
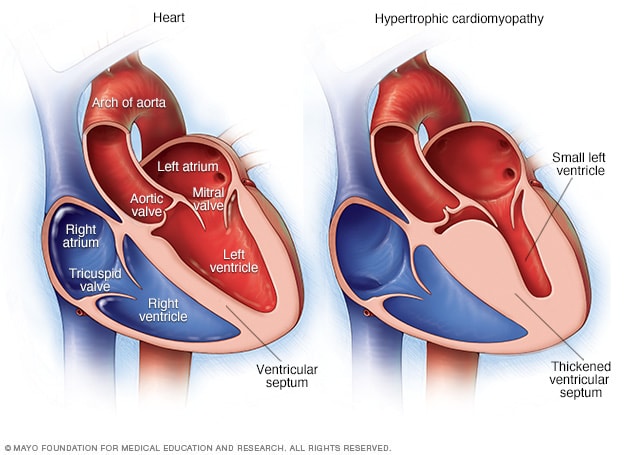
Hypertrophic cardiomyopathy
Illustrations of a regular heart (left) and a heart with hypertrophic cardiomyopathy. Note that the heart walls (muscles) are much thicker (hypertrophied) in the heart with hypertrophic cardiomyopathy.
Often the cause of the cardiomyopathy is unknown. In some people, however, it's the result of another condition (acquired) or passed on from a parent (inherited).
Certain health conditions or behaviors that can lead to acquired cardiomyopathy include:
- Long-term high blood pressure
- Heart tissue damage from a heart attack
- Long-term rapid heart rate
- Heart valve problems
- COVID-19 infection
- Certain infections, especially those that cause inflammation of the heart
- Metabolic disorders, such as obesity, thyroid disease or diabetes
- Lack of essential vitamins or minerals in the diet, such as thiamin (vitamin B-1)
- Pregnancy complications
- Iron buildup in the heart muscle (hemochromatosis)
- The growth of tiny lumps of inflammatory cells (granulomas) in any part of the body, including the heart and lungs (sarcoidosis)
- The buildup of abnormal proteins in the organs (amyloidosis)
- Connective tissue disorders
- Drinking too much alcohol over many years
- Use of cocaine, amphetamines or anabolic steroids
- Use of some chemotherapy drugs and radiation to treat cancer
Types of cardiomyopathy include:
-
Dilated cardiomyopathy. In this type of cardiomyopathy, the heart's main pumping chamber — the left ventricle — becomes enlarged (dilated) and can't effectively pump blood out of the heart.
Although this type can affect people of all ages, it occurs most often in middle-aged people and is more likely to affect men. The most common cause is coronary artery disease or heart attack. However, it can also be caused by genetic changes.
-
Hypertrophic cardiomyopathy. This type involves abnormal thickening of the heart muscle, which makes it harder for the heart to work. It mostly affects the muscle of the heart's main pumping chamber (left ventricle).
Hypertrophic cardiomyopathy can develop at any age, but the condition tends to be more severe if it occurs during childhood. Most people with this type of cardiomyopathy have a family history of the disease. Some genetic changes have been linked to hypertrophic cardiomyopathy.
-
Restrictive cardiomyopathy. In this type, the heart muscle becomes stiff and less flexible, so it can't expand and fill with blood between heartbeats. This least common type of cardiomyopathy can occur at any age, but it most often affects older people.
Restrictive cardiomyopathy can occur for no known reason (idiopathic), or it can by caused by a disease elsewhere in the body that affects the heart, such as amyloidosis.
- Arrhythmogenic right ventricular dysplasia. In this rare type of cardiomyopathy, the muscle in the lower right heart chamber (right ventricle) is replaced by scar tissue, which can lead to heart rhythm problems. It's often caused by genetic changes.
- Unclassified cardiomyopathy. Other types of cardiomyopathy fall into this category.
Risk factors
There are a number of things that can increase your risk of cardiomyopathy, including:
- Family history of cardiomyopathy, heart failure and sudden cardiac arrest
- Long-term high blood pressure
- Conditions that affect the heart, including a past heart attack, coronary artery disease or an infection in the heart (ischemic cardiomyopathy)
- Obesity, which makes the heart work harder
- Long-term alcohol misuse
- Illicit drug use, such as cocaine, amphetamines and anabolic steroids
- Treatment with certain chemotherapy drugs and radiation for cancer
Many diseases also raise your risk of cardiomyopathy, including:
- Diabetes
- Thyroid disease
- Storage of excess iron in the body (hemochromatosis)
- Amyloidosis
- Sarcoidosis
- Connective tissue disorders
Complications
Enlarged heart, in heart failure
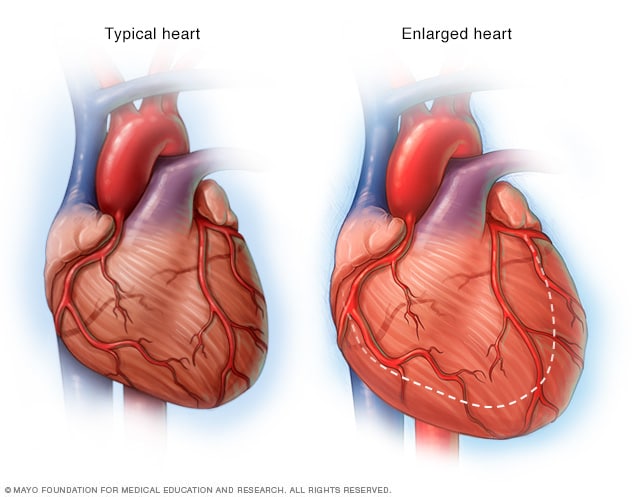
Enlarged heart, in heart failure
If the heart weakens, as it can with heart failure, it begins to enlarge. This forces the heart to work harder to pump blood to the rest of the body.
Cardiomyopathy can lead to serious complications, including:
- Heart failure. The heart can't pump enough blood to meet the body's needs. Untreated, heart failure can be life-threatening.
- Blood clots. Because the heart can't pump effectively, blood clots might form in the heart. If clots enter the bloodstream, they can block the blood flow to other organs, including the heart and brain.
- Heart valve problems. Because cardiomyopathy causes the heart to enlarge, the heart valves might not close properly. This can cause blood to flow backward in the valve.
- Cardiac arrest and sudden death. Cardiomyopathy can trigger irregular heart rhythms that cause fainting or, in some cases, sudden death if the heart stops beating effectively.
Prevention
In many cases, there's no prevention for cardiomyopathy. Let your health care provider know if you have a family history of the condition.
You can help reduce your risk of cardiomyopathy and other types of heart disease by living a heart-healthy lifestyle, including:
- Avoiding the use of alcohol or cocaine
- Controlling high blood pressure, high cholesterol and diabetes
- Eating a healthy diet
- Getting regular exercise
- Getting enough sleep
- Reducing your stress
The Mayo Clinic experience and patient stories
Our patients tell us that the quality of their interactions, our attention to detail and the efficiency of their visits mean health care like they've never experienced. See the stories of satisfied Mayo Clinic patients.