Overview
A concussion is a traumatic brain injury that affects your brain function. Effects are usually temporary but can include headaches and problems with concentration, memory, balance and coordination.
Concussions are usually caused by a blow to the head. Violently shaking of the head and upper body also can cause concussions.
Some concussions cause you to lose consciousness, but most do not.
Falls are the most common cause of concussion. Concussions are also common if you play a contact sport, such as football or soccer. Most people usually recover fully after a concussion.
Symptoms
The signs and symptoms of a concussion can be subtle and may not show up immediately. Symptoms can last for days, weeks or even longer.
Common symptoms after a concussive traumatic brain injury are headache, loss of memory (amnesia) and confusion. The amnesia usually involves forgetting the event that caused the concussion.
Physical signs and symptoms of a concussion may include:
- Headache
- Ringing in the ears
- Nausea
- Vomiting
- Fatigue or drowsiness
- Blurry vision
Other signs and symptoms of a concussion include:
- Confusion or feeling as if in a fog
- Amnesia surrounding the traumatic event
- Dizziness or "seeing stars"
A witness may observe these signs and symptoms in the concussed person:
- Temporary loss of consciousness (though this doesn't always occur)
- Slurred speech
- Delayed response to questions
- Dazed appearance
- Forgetfulness, such as repeatedly asking the same question
You may have some symptoms of concussions immediately, and some can occur for days after the injury, such as:
- Concentration and memory complaints
- Irritability and other personality changes
- Sensitivity to light and noise
- Sleep disturbances
- Psychological adjustment problems and depression
- Disorders of taste and smell
Symptoms in children
Head trauma is very common in young children. But concussions can be difficult to recognize in infants and toddlers because they can't describe how they feel. Concussion clues may include:
- Dazed appearance
- Listlessness and tiring easily
- Irritability and crankiness
- Loss of balance and unsteady walking
- Excessive crying
- Change in eating or sleeping patterns
- Lack of interest in favorite toys
- Vomiting
- Seizures
When to see a doctor
See a doctor within 1 to 2 days if:
- You or your child experiences a head injury, even if emergency care isn't required
If your child doesn't have signs of a serious head injury, remains alert, moves normally and responds to you, the injury is probably mild and usually doesn't need further testing.
In this case, if your child wants to nap, it's OK to let him or her sleep. If worrisome signs develop later, seek emergency care.
Seek emergency care for an adult or child who experiences a head injury and signs and symptoms such as:
- Repeated vomiting or nausea
- A loss of consciousness lasting longer than 30 seconds
- A headache that gets worse over time
- Fluid or blood draining from the nose or ears
- Vision or eye disturbances, such as pupils that are bigger than normal (dilated pupils) or pupils of unequal sizes
- Ringing in the ears that doesn't go away
- Weakness in the arms or legs
- Appearing very pale for longer than an hour
- Changes in behavior
- Confusion or disorientation, such as difficulty recognizing people or places
- Slurred speech or other changes in speech
- Obvious difficulty with mental function or physical coordination
- Changes in physical coordination, such as stumbling or clumsiness
- Seizures or convulsions
- Lasting or recurrent dizziness
- Symptoms that worsen over time
- Large head bumps or bruises on areas other than the forehead in children, especially in infants under 12 months of age
Athletes
Never return to play or vigorous activity while signs or symptoms of a concussion are present.
Experts recommend that an athlete with a suspected concussion not return to activities that are associated with a higher risk of another concussion while still showing concussion symptoms.
Children and adolescents should be evaluated by a health care professional trained in evaluating and managing pediatric concussions.
Experts also recommend that adult, child and adolescent athletes with concussions not return to play on the same day as the injury.
Causes
Types of concussion injuries
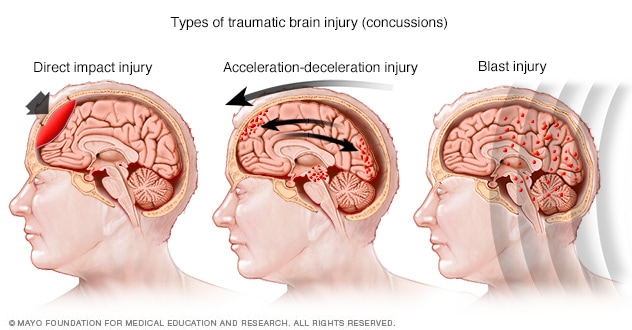
Types of concussion injuries
Common injuries that cause concussions include falls or other direct hits to the head, car accidents and blast injuries from explosions. These injuries can affect the brain in different ways and cause different types of concussions.
Your brain has the consistency of gelatin. It's cushioned from everyday jolts and bumps by cerebrospinal fluid inside your skull.
A violent blow to your head and neck or upper body can cause your brain to slide back and forth forcefully against the inner walls of your skull.
Sudden acceleration or deceleration of the head, caused by events such as a car crash or being violently shaken, also can cause brain injury.
These injuries affect brain function, usually for a brief period, resulting in signs and symptoms of concussion.
This type of brain injury may lead to bleeding in or around your brain, causing symptoms such as prolonged drowsiness and confusion. These symptoms may develop immediately or later.
Such bleeding in your brain can be fatal. That's why anyone who experiences a brain injury needs monitoring in the hours afterward and emergency care if symptoms worsen.
Risk factors
Activities and factors that may increase your risk of a concussion include:
- Falling, especially in young children and older adults
- Participating in a high-risk sport, such as football, hockey, soccer, rugby, boxing or other contact sport
- Participating in high-risk sports without proper safety equipment and supervision
- Being involved in a motor vehicle collision
- Being involved in a pedestrian or bicycle accident
- Being a soldier involved in combat
- Being a victim of physical abuse
- Having had a previous concussion
Complications
Potential complications of concussion include:
- Post-traumatic headaches. Some people experience concussion-related headaches up to seven days after a brain injury.
- Post-traumatic vertigo. Some people experience a sense of spinning or dizziness for days, weeks or months after a brain injury.
- Persistent post-concussive symptoms (post-concussive syndrome). A small proportion of people (15% to 20%) may have symptoms including headaches, dizziness and thinking difficulties that persist beyond three weeks. If these symptoms persist beyond three months, this becomes characterized as persistent post-concussive symptoms.
- Cumulative effects of multiple brain injuries. Active research is currently underway to study the effects of repeated head injuries that don't cause symptoms (subconcussive injury). At this time, there's no conclusive evidence indicating that repeated brain injuries contribute to cumulative effects.
-
Second impact syndrome. Rarely, experiencing a second concussion before signs and symptoms of a first concussion have resolved may result in rapid and usually fatal brain swelling.
It's important for athletes never to return to sports while they're still experiencing signs and symptoms of concussion.
Prevention
Some tips that may help you to prevent or minimize your risk of head injury include:
-
Wearing protective gear during sports and other recreational activities. Make sure the equipment fits properly, is well maintained and is worn correctly. Follow the rules of the game and practice good sportsmanship.
When bicycling, motorcycling, snowboarding or engaging in any recreational activity that may result in head injury, wear protective headgear.
- Buckling your seat belt. Wearing a seat belt may prevent serious injury, including head injury, during a traffic accident.
- Making your home safe. Keep your home well lit and your floors free of anything that might cause you to trip and fall. Falls around the home are a leading cause of head injury.
- Protecting your children. To help lessen the risk of head injuries to your children, block off stairways and install window guards.
- Exercising regularly. Exercise regularly to strengthen your leg muscles and improve your balance.
- Educating others about concussions. Educating coaches, athletes, parents and others about concussions can help spread awareness. Coaches and parents can also help encourage good sportsmanship.
Feb. 17, 2022